导图社区 Lipid diseases
- 54
- 0
- 0
- 举报
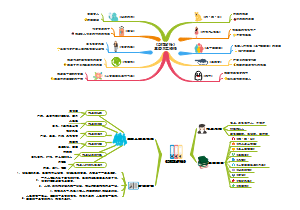
Lipid diseases
Lipid diseases:SREBP: Sterol regulatory element binding protein;SCAP: SREBP cleavage activating protein。
编辑于2022-06-08 22:56:27- fatty acids
- Transport…
- Cholesterol
- 相似推荐
- 大纲
Lipid diseases
biochemistry of lipids
Common features
energatically impact: highly reduced carbon
nonpolar that is insoluble in water (hydrophobic)
Biological functions
Energy source
fatty acids
Energy storage
triacylglycerides
Membrane structure
phospholipids
sphingomyelin
cholesterol
Vitamins
Vitamins A
Vitamins D
Vitamins E
Vitamins K
Bile salts
An aid to digestion of dietary lipid and lipid adsorption in the intestine.
Ubiquinone
part of electron transport chain
Signaling molecule
phosphatidylinositol
PIP2
PIP3
diacylglycerol
DAG
Steroid hormones
Eicosanoids
Structural divisions
By back bones
Open chian
Fatty acids
Most fatty acids have an even number of carbons, usually 14-24.
Glycerolipids (triacylglycerols/triglycerides)
Fat, plant oil
Simple triacylglycerol
all 3 fatty acids are the same
Mixed triacylglycerol
fatty acids are different
Glycerophospholipids
A phosphoric acid esterifies one of the alcohol groups of glycerol.
The phosphoric acid can attaches another group X
Glycerophospholipids are the major component of membranes
lipids compositions are tissue and organells dependent
Sphingolipids
Fused ring
Sterol lipids
Cholesterol
most common steroid in animals
essential component of cell membranes
Cholesterol derivatives
Sterioid hormones
Key regulator of gene transcription
Vitamin D
Key regulator of Ca2+ level
Bile acids
Facilitating the formation of miscelles which promotes processing of dietary fat.
Free form/esterified
The hydroxyl group can be esterified, estrified cholesterol accounts for 70% of the circulating cholesterol.
By double bonds
saturated
all carbon-carbon bonds are single bonds.
results
they pack tightly and form more rigid, organized structures.
unsaturated
contains one or more double bonds in hydrocarbon chain.
results
for membrane phospholipids
it increases the membrane fluidity
intermolecular forces are not as great as the saturated chains, and there is greater potential for motion within a membrane.
for fats
trans fat has weaker intramolecular forces due to their structures.
trans fat tends to have lower melting points than the cis fats
hydrogenation of unsaturated fatty acids
aim to produce plant derived saturated butter used in food industry
can produce many trans fats
that is why animal fats are solid under room temperature
Cis, trans and the pocision of double bonds
they will contribute to the complexities of the lipid conformations.
120° for cis bonds, 180° for trans double bonds.
naming system
normal (single-unsaturated)
Carbonyl carbon is C1
alternative (poly-unsaturated)
The methyl carbon at the end of the tail is C1
this is also called omega carbon
Position of the double bonds are indicated relitive to the C1
fatty acids and heart diseases
Omega-6 derived eicosanoids
Phospholipase A2 Cleaves Membrane lipids into Arachidonic acid.
Steroids inhibits Phospholipase A2.
Cycloxygenases(COX-1 and -2) oxidize Arachidonic acid(Omega-6 fatty acids) into Omega-6 derived Eicosanoids.
NSAIDs(nonsteroidal antiinflammatory drugs)(e.g. Aspirin, ibuprofen) inhibit cyclooxygenases.
Aspirin can acetylases an essential Ser residue in COX and inactivates it.
Steroid drug: glucocorricoids repress the synthesis of COX-2 and inhibit the action of phospholipase A2.
Omega-6 derived Eicosanoids can be
Prostaglandins
It is a pro-inflammatory signaling molecule.
Thromboxanes
It is a blood clotting signaling molecule released by damaged arteries.
It causes blood platelets to clump togather
Omega 3 fatty acids can compete with omega-6 fatty acids in the synthesis of eicosanoids.
Omega-3 derived eicosanoids do not includes thromboxanes.
Omega-3 derived eicosanoids is synthesized much more slowly than Omega-6 derived eicosanoids.
Omega-3 fatty acids reduce the incidences of heart diseases
This is why people eat fish is good for their health,
Cholesterol and diseases
Origins of cholesterol in our bodies
1. Diet
meat
eggs
diary products
2. De novo synthesis
Chemical reactions
Regulation of HMG CoA Reductase
Short-term regulation
AMP -> AMPK(AMP-dependent protein kinase) -p| HMG CoA Reductase
Over all: AMP --| HMG CoA Reductase
Interptrtation
The cellular energy availability controles the synthesis of Cholesterol
Longterm regulations by proteolysis and Transcriptional regulations
SREBP: Sterol regulatory element binding protein
SCAP: SREBP cleavage activating protein
Cholesterol -> Insig -| {SCAP]-[SCREBP}
Cholesterol binds and activates Insig, insig associates with SCAP-SCREBP complex by interacts with SCAP, this interaction inhibits the transport protein from binding to SCAP
SREBP Reg domain interacts with SCREBP
In ER
Cholesterol -> Insig -| Transport protein -(location change from ER to golgi apparatus)> {SCAP][SCREBP}
Transport protein binds directly with SCAP
In Golgi apparatus
1. Serine protease -(cleavage)> SCREBP
The specific sites and results of the proteolysis can be seen on the picture.
2. Zn++ -> metalloprotease -(cleavage)> free SCREBP DNA-binding domain ->o-> HMG-CoA Reductase
Release the DNA binding domain.
Another mechanism
Cholesterol -> Insig(it is normally associating with ubiquitinating enzymes) -> Ubiquitinating enzymes +u(first binds) HMG-CoA reductase --> peoteosome degradation of HMG-CoA reductase
Interpretation
Cholesterol --> proteosome degradation of HMG-CoA reductase
Cholesterol --| Expression of HMG-CoA Reductase
Those are 2 feed back inhibition mechanisms
HMG CoA reductase is the rate limiting enzyme in cholesterol de novo synthesis
Statins inhibits HMG-CoA reductase, and it will reduces blood cholesterol
Statins is the competitive inhibitor, Statin mimics mevalonate,mevalonate is the transition state analogs of the HMG-CoA reductase
The sythesis of cholesterol consumes ATP and NADPH in cytosol
All the carbons in the Cholesterol are derived from the acetyl group in actetyl-CoA
Mostly in liver
80% in liver
some in extrahepatic tissues
10% in intestine
5% in skin
Liver stores cholesterol , Usage of cholesterol in liver:
Export by HDL and VLDL
Secreted in biles
Cholesterol converted bile salts/acids
Free cholesterol in bile
Usage of cholesterol
Execssive cholesterol
Exessive cholesterol circulates and accumulates in boold vessels, this thickens the antery wall(atherosclerosis).
Atherosclerosis will obstruct blood flow.
Essesive blood cholesterol also causes coronary heart diseases
production of bile salts and steroids
compartment for plasma membranes
How to reduce blood cholesterol levels
1. use Statins to competatively inhibits HMG-CoA reductase
2. eat plant sterols and stanols
rich in Yogurts and margarines
plant sterols compete with choleserol absorptions in intestine.
it occupies the mixed micelles, and itself is very poorly obsorbed.
This reduces the absorption of dietary cholesterol, and the liver can removes the harmful cholesterol from the blood.
3. use bile sequestering agents
it binds bile acids.
it utilizes more cholesterol to make bile acids.
Transportation of lipids in blood
Basics about lipoprotein
lipoprotein varies among sizes
Cholesterol components generally make the lipoproteins bigger
Appoprotein(the protein parts of the lipoprotein) contributes to both solubility and signaling of lipoproteins
Solubility
The apoproteins are highly polar, which provides an interface between polar water molecules and non-polar lipid molecules.
You may find phospholipids here provide the similar role as the interface.
signaling
apoproteins on the surface of lipoproteins provide distinct identities for different lipoproteins
VLDL
IDL
LDL
HDL
all of these have different surface signalings
Roles of lipoproteins
An overview
You can see HDL has a very important role here, it transport lipids(cholesterols) from peripheral tissues back to liver for its degradation(converte to bile salts)
You can see LDL generally acts as opposite as HDL
The lipids they are transporting are mostly cholesterols
High blood cholesterols are associated with atherosclerosis and cardiovascular diseases
high LDL levels also strongly correlate with atherosclerosis and cardiovascular diseases
Generally
atherosclerosis is due to the overload of the cholesterol transport pathway
it could due to high cholesterol intake, or reduction of functional LDLR
The reduction of functional LDLR is the cause of a familial hypercholesterolemia
So LDL is often called bad cholesterol
high HDL levels often reduces the risk of those diseases
So HDL is often called good cholesterol
High saturated fatty acids and trans fatty acids increase LDL levels
We may not know why
VVLDL(Chylomicrons)
TAG
intestine -> Periferal tissues/liver
(diatery TAG)
VLDL
TAG
liver -> tissues
LDL
TAG
tissues -> liver
Cl
liver -> tissues
IDL
TAG
liver -> tissues
sometimes tissues -> liver
HDL
Cl
tissues -> liver
Acronyms used
Cl
cholesterol
Tag
triacylglycerol
or fats
Receptors and Enzymes for lipoproteins
Chylomicrons activate LPL(lipoprotein lipase). LPL hydrolyzes TAG (triacylglycerol), and the resulting glycerol and FFA (free fatty acids) are absorbed by peripheral/adipose tissues for energy usage/storage
interpretation: chylomicrons will activate an enzyme that will readily consumes the TAG component within it.