导图社区 Cancer
- 23
- 1
- 0
- 举报
Cancer
Cancer:Drugs/antibodies targeting Ras family or p53 and other oncogenes or tumour suppressor genes。
编辑于2022-06-08 22:01:31- Cancer
- 相似推荐
- 大纲
Cancer
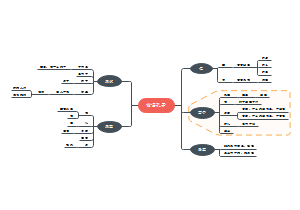
Genetics of cancer
A polygenic/oligogenic disease
200 types of cancer with 300 genes involved
Requires multiple mutations to develop a full cancer cell
20% in germ-line cells
90% in somatic cells
The heridity cases are only 5%!
95% are sporadic
every one could be potentially having this dreadful disease....
Oncogenes
Proto-oncogenes encode proteins that promote cell growth and divisions.
When proto-oncogenes get mutated, they become oncogenes.
Gain of function mutation from proto-oncogenes
>70 identified
dominance
Correspond
Viral orignin
Rous Sarcoma Virus, RSV
scr(v-ongogene) can resembles cellular
Growth Factors
v-sis (Simian Sarcoma) oncogene: a protein that strongly resembles a protein called PDGF (platelet-derived growth factor)
Growth Factor receptors
e.g. v-erbB (Avian Erythroblastosis Virus) oncogene: encodes a protein that resembles part of the EGF (Epidermal Growth Factor) receptor
Signal Transducers: e.g. ras oncogene
Transcription Factors
e.g. fos and jun. The Fos and Jun proteins constitute the transcription factor AP-1, that activate genes in response to growth factor stimulation
Tumor supressor genes
Tunor supressor genes encode proteins that restrain cell growth and divisons.
Loss of function
recessive
loss of heterozygosity (LoH),
The deletion of a wild-type allele in an individual at heterozygous TSG locus causes a loss of heterozygosity (LoH), resulting in no functional TSG protein being made, and loss of the capability to prevent cancer formation
p53
mutated in 50% of all cancers
•In erythroleukemia induced by the Friend virus, p53 was inactivated (no expression/truncated/mutated)
•When co-transfected with Ha-ras, less tumors were formed (anti-oncogenic)
•In many cancers, there is LoH of the Chr17 (where p53 gene is)
•Mutations in p53 were found in the germ-line cells of Li-Fraumeni patients
Gatekeepers genes
inhibit cell growth or promote cell death
e.x. APC protein controls cell proliferation in the colon
When the APC gene is mutated, β-catenin is not degraded and the levels remain high, β-catenin regulates proliferation of the colon cells
five to seven specific genes are required to bring about malignant growth
The hereditary case acounts for 5% colon cancer, it has one mutation copy of APC
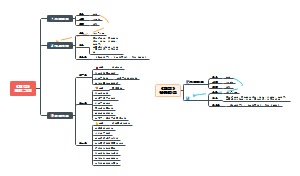
Caretaker genes
help maintain the integrity of the genome. DNA repair genes are examples of caretaker genes
Like HNPCC
DNA repair mechanisms
Nucleotide excision repair(NER)
XP (Xeroderma Pigmentosum)
due to defective in any of the 30 proteins involved in NER
XP cells: extreme sensitivity to UV radiation
–Increased chromosome abnormalities
•T-T/C-T/C-T dimers
•Nucleotide crosslinks
•Nucleotide-specific side group modifications
–Lowered ability to repair UV-damaged DNA
Replication error repair/MisMatch repair (MMR)
Ataxia Telangiectasia (AT)
Autosomal recessive: ATM gene
HNPCC results from an inherited defect in one copy of a mismatch repair gene (MSH2, MLH1, MSH6, PMS1, PMS2 and others)
HNPCC individuals have dramatically increased risk of colon, ovarian, uterine and kidney cancers
Tumor develops by loss of heterozygosity
Homologous recombination repair(HRR)
Part of double strand break repair
Fanconi Anemia (FA)
Defect in repair of DNA damage known as interstrand cross-links (ICLs) via HRR mechanism: ~15 genes (Genetic heterogeneity)
•FA core complex activates FANCD2&FANCI HRR complex
Breast Cancer (BRCA1 & BRCA2)
5% of breast cancer is due to this hereditary predisposition
tumor suppressor genes
•Most common mutation in BRCA1 is the deletion of two adjacent bases (resulting in a frameshift mutation and truncation of the protein)
•Predisposition inherited as an autosomal dominant
•However, both BRCA1 and BRCA2 show incomplete penitrance
BRCA2 has a direct role in HRR, BRCA1 also has other roles including cell cycle control
•A critical protein in HRR is RAD51 which is the functional homologue of RecA protein in E. coli
just the singgle strand binding proteins
•After DNA damage, RAD51 protein forms foci in the nucleus which are the sites of HRR
•Both BRCA1 and BRCA2 proteins colocalize to the RAD51 foci
BRCA1 and BRCA2 are not mutated in sporadic breast cancer
Tumour cell lines with mutations in both copies of either BRCA1 or BRCA2 exhibit increased sensitivity to DNA damaging agents
•A lack of DNA repair by HRR leads to genomic instability
How can we treat cancer?
Conventional therapies
Surgical removal
Chemotherapy, radiotherapy
Chemotherapy Targets DNA, RNA and protein to disrupt the cell cycle in rapidly dividing cancer calls (causing DNA damage and apoptosis)
Lack selectivities
Damage normal cells
New therapies
Drugs/antibodies targeting Ras family or p53 and other oncogenes or tumour suppressor genes
Can be Cancer type specific
High selectivities
Damage less normal cells
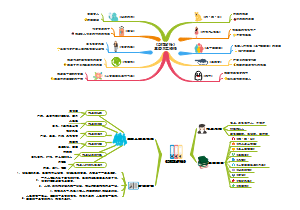
Are more people easier to get cancer now?
For some type of cancer, it's effected by some historical event
And male/female are really different in the incidence of different cancers
The Mortality is decreased more rapid than the incidence
Also emergence of different cancers show regional specificity
this reflects the consequences of people's life styles
What habits can lead to cancer?
Smoking
Obesity
But it will make you more likely to survive after developing cancer
Phyisical inactive
poor nutrition
Most of carcinogens are mutagens
How many people dead from cancers?
One in 4 deaths in the United States is due to cancer.
In duration of 4 years, 0.5% of population would have cancer, and 0.2% of the population will die by cancer.
What cells develop cancer?
totally 300 cell types in human
The daily dividing cells
innerskin
blood
intestinal lining
The cells divide rapid after damages
liver cells
Cells proliferate in response to particular bacteria & viruses
immune cells
Cells terminally differentiated, never divide
most neurons
surface skin
General Classification of cancers (based on tissue origins)
carcinomas
Cells that line organs and form part of the skin
85%
sarcomas
Cells of connective, bone, or muscle tissues
2%
lymphomas
White blood cells of the spleen or lymph nodes
5%
leukemias
White blood cells (leukocytes) of the blood system
3%
adenocarcinomas
Cancers of glandular tissues
5%
astrocytomas
gliomas or Non-neuronal cells of the brain
myelomas
Plasma cells
Cancer cells have several developmental stages.
mutations respond for the transitions between stages.
This is why Cancer usually occurs in old people, because they get successfully accumulated those mutations
Cancer can be developed if One cell gets all of those neccesary mutations
Normal stages of cancer
Normal cells -> Lump -> Localized cancer -> carcinoma
What are tumours
Simple defination
A group of normal cell derived, unregulated deviding cells
Sub divide into cancer and benign tumour
Metastasis
invasion and spread of cells from the site of origin to other sites in the body
50% patients have metastasis when they visit doctors
Cancer is metastatic tumour, and it can breaks basement membrane
Benign tumour is not metastatic(self contained)
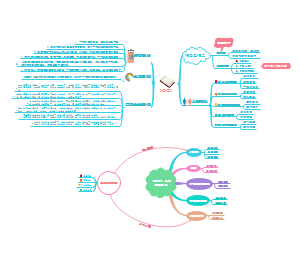
How the cells lose control on their growth?
An obvious and superficial answer is that the number of newly devided cells is greater than the number of cells undergo appoptosis.
The specific molecular insights of cancer(hall marks)
1.growth factor autonomy
Growth factors are normally act as an extracellular permission for all the cells to grow.
Mutations in cancer short circuit growth factor pathways, it leads to cancer some extend independent of extracellular growth factor to grow.
2. Evasion of growth inhibitory signals
Extracellular inhibitory signals normally act as a guardian for all the cells to grow as well.
Mutations in cancer can interfer with inhibitory signal's intracellular pathways, this finally leads to the iresponssiveness to the extracellular inhibitory signals.
3. avoiding immune destructions
Cancer cells may be invisible for immune systems, or they may secret some molecules to interfer normal immune responses.
4. unlimited replicative potential
Cancer cells aquire immortalities, means they can divide after 40 cell cycles, which is the limit of most normal cells
this might due to the limitation of their telomere length
When telomere repreats shorten below a limit after multiple rounds of cell divisions, the cell would undergo appoptosis.
somatic cells do not have telomerase, telomere will completely lost after 40 rounds of divisions, and the sisterchromatids will fuse by translocation mutation, this will breaks the chromosome during division, and it will leads to appoptosis.
Cancer cells maintain the length of their telomeres, this might due to they maintain the high level expression of telomerase.
Evidence
the transfection of expressing telomerase in normal cell culture will lead cells to immortal
Telomerase is a reversetranscriptase that can elognates DNA telomeres based on RNA templates.
5. Tumour-promoting inflammation
All tumour tissues contain immune cells that can promote inflammation.
Those cells can release growth factors, angiogenesis enzymes, invasion enzymes, and mutagenic oxygen species.
6. Invation and metastasis
Invation and metastasis are major causes of cancer death.
Mutations may affect the activity and/or levels of enzymes involved in invasion or molecules involved in cell-cell or cellular-extracellular adhesion.
7. Angiogenesis
Blood vessels should not further grow in normal adult.
Cancer cell induce angiogenesis, the newly generated blood vessels support tumour survival and expansions.
Altering the balance between angiogenic inducers and inhibitors can activate the angiogenic switch.
8. Genome instability and mutation
Failure of DNA repair mechanisms can increases the chance getting the mutations of other hall marks.
9. Evasion of cell death
DNA damages or other signals can trigure the death of normal cells.
Cancer cells can evade apoptosis.
10. Reprogramming energy metabolisms
Elevated energy metabolisms allow cancer cells to continue their divsion and growth.
Glycolysis is unconditionally processed in cancer cells, becauce tumour tissues require generated ATP and other metabolism products to growth.
Cellular compartments changes
Generally, the nucleus of cancer cells are enlarged, with multiple nucleoli and mau have multiple nuclei. the chromatin remins coarse.
Cultural mophology/condation changes
Cancer cells lose contact inhibitions
Contact inhibition means stop growth when the cell fill the dish.
Cancer cells can grow in conditions of low serum
Cancer cells are anchoring independent
Cancer cells has round morphologies
normal cells has flat and extented morphologies