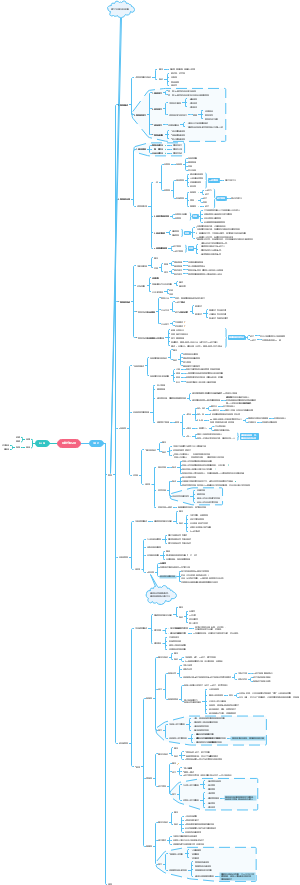
导图社区 Alevel 生物 第十章 Infectious diseases
- 1.3k
- 25
- 13
- 举报
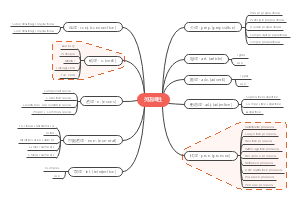
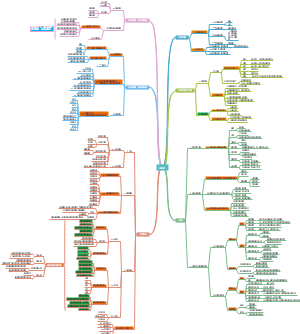
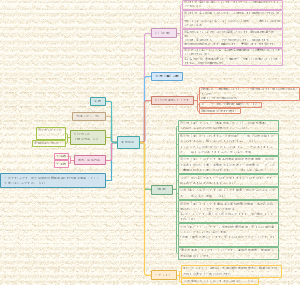
Alevel 生物 第十章 Infectious diseases
Alevel 生物 知识结构导图第十章传染病。内容包括:肺炎、疟疾、结核病、艾滋病等常见传染病的病原、传播、治疗和防控,抗生素及其耐药性等
编辑于2021-06-10 11:30:52- 国际教育
- 相似推荐
- 大纲
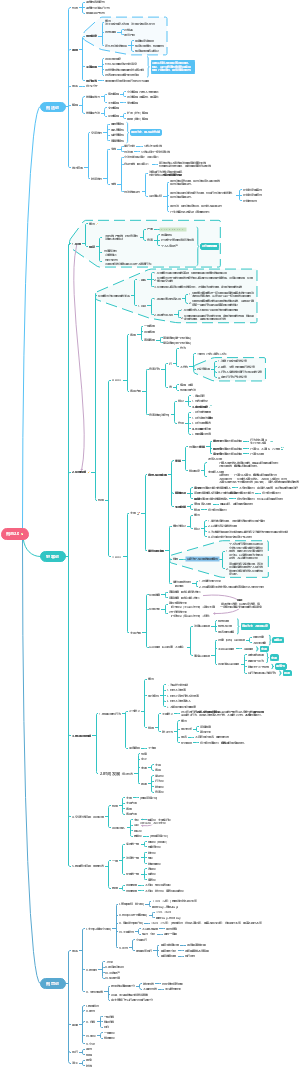
Infectious diseases
Worldwide importance of infectious diseases
Infectious diseases are diseases that are caused by organisms known as pathogens
non-infectious diseases
long-term degenerative diseases:lung cancer and COPD
Inherited or genetic diseases:cystic fibrosis and sickle cell anaemia
deficiency diseases:caused by malnutrition and mental diseases
Infectious diseases
affect us for a short period of time:the common cold, measles and influenza; last a much longer time: tuberculosis (TB), HIV/AIDS;
spread by direct contact/ transmitted indirectly from person to person
carriers:people spread a pathogen but lack symptoms
the transmission cycle:The way in which a pathogen passes from one host to another
Vaccination is a major control measure; it works by making us immune so that pathogens do not live and reproduce within us and do not then spread to others
endemic:Diseases that are always in populations
incidence:the number of people who are diagnosed over a certain period of time
prevalence:the number of people who have that disease at any one time
epidemic: a sudden increase in the number of people with a disease
pandemic: an increase in the number of cases throughout a continent or across the world
mortality: the death rate

Cholera
Transmission of cholera
the bacterium Vibrio cholerae


Treating cholera
make a quick recovery
a solution of salts and glucose given intravenously to rehydrate the body/oral rehydration therapy
It is important to make sure that a patient’s fluid intake equals fluid losses in urine and faeces
to maintain the osmotic balance of the blood and tissue fluids
Preventing cholera
In developing countries,cholera is endemic are West and East Africa and Afghanistan
almost unknown in the developed world
Health authorities always fear outbreaks of cholera and other diarrhoeal diseases following natural disasters.
Strains of cholera
O1 ‘El Tor’
O139 -- for an eighth pandemic
Tuberculosis(TB)
Transmission of TB
TB is caused by either of two bacteria, Mycobacterium tuberculosis and Mycobacterium bovis


about 30% of the world's population is infected with TB without showing any symptoms of the infection; people with this inactive infection do not spread the disease to others
They have a persistent cough and, as part of their defence, cells release hormonelike compounds, which cause fever and suppress the appetite
lose weight and often look emaciated
TB is now the leading cause of death among HIV-positive people
The HIV pandemic has been followed very closely by a TB pandemic
1. TB is spread when infected people with the active form of the illness cough or sneeze and the bacteria are carried in the air in tiny droplets of liquid 2. The form of TB caused by M. bovis also occurs in cattle and is spread to humans in meat and milk
The incidence in such areas is as high as in less economically developed countries.
1.some strains of TB bacteria are resistant to drugs; 2. the HIV/AIDS pandemic 3.poor housing in inner cities and homelessness; 4. the breakdown of TB control programmes; partial treatment for TB increases the chance of drug resistance in Mycobacterium.

Treating TB
samples of the sputum from their lungs are collected for analysis
patients should be isolated while they are in the most infectious stage
Drug-resistant TB
Antibiotics act as selective agents killing drug-sensitive strains and leaving resistant ones behind
Drug resistance occurs as a result of mutation in the bacterial DNA. Mutation is a random event and occurs with a frequency of about one in every thousand bacteria.
People who do not complete a course of treatment are highly likely to infect others with drug-resistant forms of TB.
DOTS (direct observation treatment, short course) making sure that patients take their medicine regularly for six to eight months. (isoniazid and rifampicin)
MDR-TB(Multiple-drug-resistant ) strains of TB are resistant to at least the two main drugs used to treat TB ( resistant to five of the major drugs used to treat the disease)
Extensively (or extremely) drug-resistant TB (XDR-TB) are resistant to firstline drugs and to the drugs used to treat MDR-TB.
Preventing TB
Contact tracing and the subsequent testing of contacts for the bacterium are essential parts of controlling TB
The only vaccine available for TB is the BCG vaccine -- protects up to 70–80% of people who receive it
cattle are routinely tested for TB and any found to be infected are destroyed. TB bacteria are killed when milk is pasteurised.
Measles
Trasmission
one of the most contagious diseases
Measles is caused by a virus which enters the body and multiplies inside cells in the upper respiratory tract (nasal cavity and trachea).
no symptoms for 8–14 days after and then a rash appears and a fever develops; about ten days the disease clears up and there are rarely any complications.
among malnourished children living in overcrowded conditions, measles is a serious disease and a major cause of death.
When people infected with measles sneeze or cough they release droplets containing many millions of virus particles
There are estimated to be over 20 million cases of measles worldwide each year, most of which are in Africa, South-East Asia, India, Pakistan Bangladesh and some countries of the Middle East.
Treatment
Treatment involves bed rest and taking medicines to lower the fever; there are no specific medicines for measles.
The death rate from the disease has fallen from 630 000 in 1990 to 158 000 in 2011, largely as a result of a mass vaccination programme
Antibiotics
How antibiotics work
An antibiotic is a drug that kills or stops the growth of bacteria, without harming the cells of the infected organism
Antibiotics are derived from living organisms; Other antimicrobial drugs such as isoniazid are synthetic
Antibiotics interfere with some aspect of growth or metabolism of the target bacterium
1. synthesis of bacterial cell walls 2. activity of proteins in the cell surface membrane 3. enzyme action 4. DNA synthesis 5. protein synthesis

eg: Penicillin
prevents the peptidoglycan chains from linking up, but the autolysins keep making new holes in the cell walls of bacteria

Some types of bacteria are not sensitive to particular antibiotics: for example, penicillin is not effective against M. tuberculosis
antivirals
are used to control viral infections
Antibiotic resistance
1. the bacterium has a gene that codes for an enzyme that catalyses the breakdown of antibiotics. 2. Proteins in the membranes of other species of bacteria can inactivate antibiotics so they have no effect 3. bacterial membranes also have proteins that pump out antibiotics if they enter the cytoplasm 4.the antibiotic simply cannot bind to the intended site of action
Bacteria that are sensitive to an antibiotic are described as being susceptible to that antibiotic. They may become resistant if they gain a gene coding for a protein that protects them from the antibiotic.
Penicillin has a structure that can be broken down by β-lactamase (penicillinase) enzymes
Pathogenic bacteria that have become resistant to penicillin have often done so because they have acquired the genes that code for these enzymes.
vertical transmission
Genes for antibiotic resistance often occur on plasmids, which are small loops of double-stranded DNA
Plasmids are quite frequently transferred from one bacterium to another, even between different species

horizontal transmission
The more we misuse antibiotics, the greater the selection pressure we exert on bacteria to evolve resistance to them.
Bacteria living where there is widespread use of antibiotics may have plasmids carrying resistance genes for several different antibiotics, giving multiple resistance.
Choosing effective antibiotics
Antibiotics should be chosen carefully
Testing antibiotics against the strain of the bacterium isolated from people ensures that the most effective antibiotic can be used in treatment.
there is a constant search for new antibiotics
Clearly we should try to reduce the number of circumstances in which bacteria develop resistance to antibiotics
1. using antibiotics only when appropriate and necessary; not prescribing them for viral infections 2. reducing the number of countries in which antibiotics are sold without a doctor's prescription 3. avoiding the use of so-called wide-spectrum antibiotics and using instead an antibiotic specific to the infection (known as narrow spectrum) 4. making sure that patients complete their course of medication 5. making sure that patients do not keep unused antibiotics for self-medication in the future 6. changing the type of antibiotics prescribed for certain diseases so that the same antibiotic is not always prescribed for the same disease 7. avoiding using antibiotics in farming to prevent, rather than cure, infections.
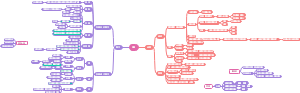
Malaria
Transmission of malaria
one of four species of the protoctist Plasmodium




Treating malaria
Anti-malarial drugs
quinine
chloroquine
prophylactic drugs -- inhibits protein synthesis and prevents the parasite spreading within the body
Chloroquine resistance is widespread in parts of South America, Africa and New Guinea
proguanil
prophylactic - inhibiting the sexual reproduction of Plasmodium inside the biting mosquito
mefloquine
expensive and sometimes causes unpleasant side-effects
Resistance to mefloquine has developed notably in the border regions of Thailand
The antibiotic doxycycline
prophylactic
artesunate
used in combination with mefloquine to treat infections of P. falciparum
Preventing malaria
3 main ways to control
1.reduce the number of mosquitoes;2.avoid being bitten by mosquitoes;3.use drugs to prevent the parasite infecting people.
2 biological control measures
stocking ponds, irrigation and drainage ditches and other permanent bodies of water with fish which feed on mosquito larvae
spraying a preparation containing the bacterium Bacillus thuringiensis, which kills mosquito larvae but is not toxic to other forms of life.
The best protection against malaria is to avoid being bitten
Worldwide control of malaria
In the 1950s, the World Health Organization (WHO) coordinated a worldwide eradication programme-- not generally successful
2 main reason
Plasmodium became resistant to the drugs used to control it
mosquitoes became resistant to DDT and the other insecticides that were used at the time
Acquired immune deficiency syndrome (AIDS)
Transmission of HIV
AIDS is caused by the human immunodeficiency virus (HIV)


HIV is a retrovirus; The virus infects and destroys cells of the body’s immune system(helper T cells); allowing a range of pathogens to cause a variety of opportunistic infections
AIDS is not a disease; it is a collection of these opportunistic diseases associated with immunodeficiency caused by HIV infection.
spread by intimate human contact (direct exchange of body fluids); no vector ; unable to survive outside the human body
sexual intercourse, blood donation and the sharing of needles used by intravenous drug users, from mother to child across the placenta and, more often, through the mixing of blood during birth

1. 70% of the world's deaths from AIDS occur in Africa. 2. In 2007 it was estimated that 15 million people had died of HIV/AIDS in sub-Saharan Africa since the beginning of the pandemic. 3. 25% of the adult population of Botswana is infected with HIV. 4. Between 15% and 25% of people aged 15–49 in Botswana and Zimbabwe are infected with HIV. 5. Over 16 million children are estimated to have lost one or both parents to AIDS; in some places this is 25% of the population under 15. 6. The prevalence of HIV among women attending antenatal clinics in Zimbabwe was around 20% in 2012. 7. A large proportion of women in Rwanda are HIV positive following the use of rape as a genocidal weapon in the civil war of the early 1990s. 8. The average life expectancy in South Africa dropped from 65 to 55 during 1995–1999.
after infection
there may not be any symptoms until years later
HIV positive but does not have AIDS
opportunistically develop to create AIDS
Two of these are caused by fungi: oral thrush caused by Candida albicans, and a rare form of pneumonia caused by Pneumocystis jiroveci
As and when the immune system collapses further
less effective in finding and destroying cancers.
eg: Kaposi's sarcoma, cancers of internal organs, dementias
Treating HIV/AIDS
There is as yet no cure for AIDS and no vaccine for HIV
Drug therapy can slow down the onset of AIDS quite dramatically
expensive and have a variety of side-effects
Preventing HIV/AIDS
difficult to control
long latent stage
The virus changes its surface proteins, which makes it hard for the body’s immune system to recognise it
public health measures are the only way to stop the spread of HIV
Condoms, femidoms and dental dams
the rate of HIV infection across the world decreased by 25% between 2001 and 2009.
Contact tracing
If a person who is diagnosed as HIV positive is willing and able to identify the people whom he or she has put at risk of infection by sexual intercourse or needle sharing, then these people will be offered an HIV test.
1.explain what is meant by infectious and noninfectious diseases 2.name the organisms that cause some infectious diseases 3.explain how cholera, measles, malaria, TB and HIV/AIDS are transmitted 4.discuss the ways in which biological, social and economic factors influence the prevention and control of cholera, measles, malaria, TB and HIV/AIDS 5.discuss the factors that influence global patterns of malaria, TB and HIV/AIDS 6.outline how penicillin acts on bacteria and why antibiotics do not affect viruses 7.explain how bacteria become resistant to antibiotics 8.discuss the consequences of antibiotic resistance and how we can reduce its impact